Bones don’t scream. They don’t throb. They wait. You don’t feel your bones weakening until the silence becomes a kind of pressure. Not pain. Just fatigue. A hesitancy in your steps. A stiffness you didn’t notice before.
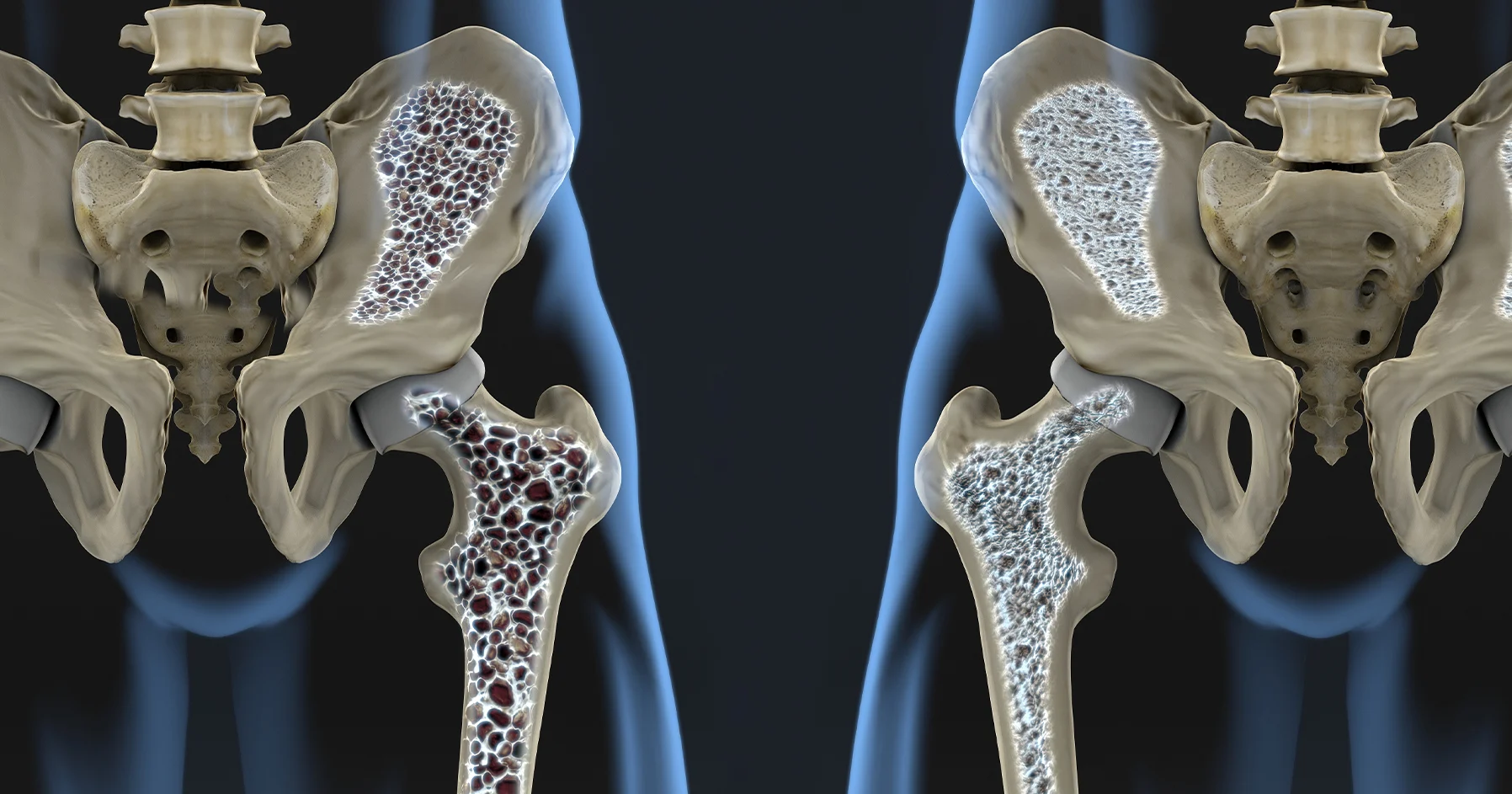
And while you stretch, rest, walk—your bones quietly lose more than strength. They lose density. Structure. Memory. This happens slowly. Without drama. Without injury.
What causes it isn’t just age. Or calcium. It’s hormonal. Endocrinology isn’t the first place people look. But it’s where the story begins.
Hormones shape how bones live, repair, and disappear
Bones aren’t bricks. They shift daily. They grow and fade in rhythm. Hormones shape how bones live, repair, and disappear. That rhythm starts with the endocrine system.
Estrogen slows down bone loss. Testosterone supports density. Growth hormone encourages rebuilding. Cortisol, when high, tears it all down.
One imbalance, one missing signal, and the body changes its instructions. It begins pulling from the bones. And the bones obey, even when it hurts them.
Estrogen doesn’t just affect cycles—it holds bone tissue in place
After menopause, something soft begins to erode. Estrogen doesn’t just affect cycles—it holds bone tissue in place. When levels drop, bones become vulnerable.
Osteoclasts—the cells that break down bone—become louder. More active. The builders, osteoblasts, fall behind. And density begins to slip.
This is why fractures become more common. Not because of trauma. But because of time. And the slow retreat of a hormone once felt in every cell.
Thyroid hormones speed everything—even the wrong things
When the thyroid is overactive, the body rushes. Heart, metabolism, digestion. But bones pay too. Thyroid hormones speed everything—even the wrong things.
Bone turnover increases. But formation can’t keep up. The scaffolding weakens. The surface hardens, but underneath, it hollows. That’s how fragility begins.
Even subclinical hyperthyroidism—too subtle to feel—can push bones toward loss. Slowly. Invisibly. Until a fall reveals what tests never showed.
Cortisol doesn’t just respond to stress—it strips strength from the center
Stress is silent, but chronic. It lingers. And cortisol responds. Over time, that response becomes toxic. Cortisol doesn’t just respond to stress—it strips strength from the center.
It reduces calcium absorption. Inhibits bone formation. Raises resorption. And the longer it lingers, the more permanent the damage.
Even people who never feel “stressed” show signs. Because cortisol doesn’t need panic to rise. It only needs pressure. Unrelenting. Invisible. Daily.
Parathyroid hormones decide what calcium stays and what leaves
Calcium doesn’t stay in bone by accident. It stays because hormones tell it to. Parathyroid hormones decide what calcium stays and what leaves.
When too high, they pull calcium into the blood. The bones lighten. When too low, they lose the signals needed to regulate density. Both paths lead to weakness.
This isn’t about diet. You can drink all the milk in the world. But if the signaling is wrong, the bones lose what they need most—direction.
Vitamin D works like a quiet messenger between sunlight and skeleton
You walk outside. You think about your skin. But your bones listen too. Vitamin D works like a quiet messenger between sunlight and skeleton.
It helps absorb calcium. Helps mineralize bone. Helps regulate parathyroid function. Without enough, the chain breaks. And bones begin to speak in cracks.
Low vitamin D doesn’t hurt at first. It just steals resilience. One step at a time. Until fractures arrive from movements that once felt ordinary.
Testosterone decline isn’t just about energy—it’s about architecture
Men often ignore it. Blame aging. But when testosterone falls, the bones feel it. Testosterone decline isn’t just about energy—it’s about architecture.
It maintains density. Mass. Repair. When levels fall, the internal scaffolding weakens. Posture changes. Strength fades. And injuries don’t recover.
Replacement therapy helps. But only when monitored. Because hormones build slowly. And the wrong dose can cause as much loss as the imbalance itself.
Insulin doesn’t just control sugar—it talks to bone too
People with diabetes often develop fractures. But not just from weight or circulation. Insulin doesn’t just control sugar—it talks to bone too.
It helps regulate bone formation. It influences mineralization. In resistance, bones lose that message. They grow brittle. Fragile. But silently.
This is why metabolic health and bone health intersect. Because every hormone echoes somewhere else. Even in the skeleton.
Bone density scans don’t tell the full story—but they start the conversation
You get a scan. Numbers come back. You’re in a range. But it’s not about the score. Bone density scans don’t tell the full story—but they start the conversation.
Because bones are more than numbers. They’re living tissues. Responding to signals, stress, sleep, and hormones. Every year. Every day.
Understanding that link helps more than calcium ever could. Because when the root cause is hormonal, the solution needs to be, too.